1 pixel (Pixel) and voxel (Voxel)
Pixel is the basic unit that constitutes an image, that is, the smallest independent information unit that an image can be decomposed into. Because the image is two-dimensional, the pixel does not have the concept of "thickness", and its biggest feature is a two-dimensional concept. Voxel refers to the volume unit corresponding to the pixel. The difference from the pixel is that the voxel is a three-dimensional concept with thickness differences, and the layer thickness corresponding to the image is the "height" of the voxel.
2 Matrix
Each image is composed of a different number of pixels. The number of pixels is usually represented by a matrix, which refers to the number of pixels in each row and each column in the rectangular area of the image, such as 256*256, 512*512, etc. In the case of the same field of view, the larger the number of matrices, the smaller the pixels and the clearer the image.
The number of CT image matrices is often the same in both the row and column directions, but it can also be different in other types of images, such as 192*256 image matrices.
3 CT value
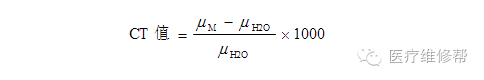
It is known from the principle of CT that different tissues have different attenuation coefficients μ for X-rays. However, in clinical use, for more convenience, the attenuation coefficient is not used directly, but the ratio of the attenuation coefficient of different tissues to water is used. The calculation formula for the CT value of tissue M is as follows:
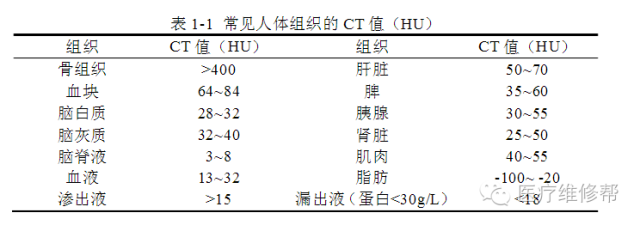
It can be seen from the above table that the higher the tissue density, the higher the CT value. Through the CT value, we can quantify the X-ray absorption coefficient of the tissue and reflect the density difference of different tissues; once a certain tissue has a lesion, the CT value of the lesion can be measured to assist in determining the composition and nature of the lesion. However, it should be pointed out that the CT value is not constant and will change due to factors such as X-ray hardening, power supply conditions, scanning parameters, temperature, and adjacent tissues. Therefore, a reasonable judgment must be made in the diagnosis.
4 window width (Window Width, WW) and window level (Window Level, WL)
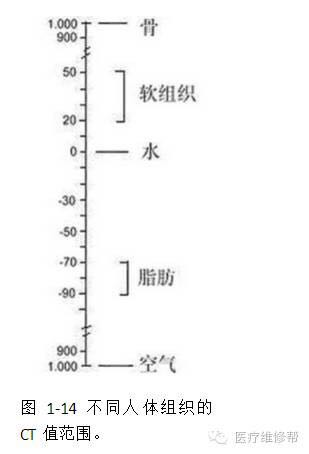
Through the concept of CT value, it is known that the density of human tissues is quite different: the lungs contain a lot of air, and the CT value is close to -1000; bones contain high-density minerals, and the highest CT value is close to +1000. The change range is only excluding the decimal point, and there is a change of 2000 HU (Figure 1-14). The grayscale changes on the display that the human eye can distinguish are about 128. In order to improve the resolution of tissues with small density differences, window technology is introduced in the display process of CT images, that is, through the setting of window level and window width, targeted observation of specific parts and tissues, highlighting structures of interest Contrast and level in the image.
Window width (WW) refers to the CT value range set to best display the structure of interest. The CT values above and below this range are displayed in completely white or black tones, that is, the difference in CT values outside this range will be displayed on the image unable to display. The midpoint of the window width range is the so-called window level (WL), usually it should be the CT value corresponding to the best displayed structure of interest, which is set as the center of the window width. For example, the CT value of the brain parenchyma is about 35 HU, and the CT value of most intracranial lesions varies from -30 to +100 HU. Therefore, the window level of the head window is selected at 35~40HU, and the window width range is selected at about 80~100HU (the specific value will be slightly different due to different equipment and habits). Such a head window setting is conducive to the observation of the brain. For the observation of the skull, it is necessary to choose a bone window with a window level of 700 HU and a window width of about 2000 HU.
In a CT image, if the window width is reduced, the difference between different tissues will be highlighted, and the contrast of the image will increase, but it looks rough. The advantage of this is that lesions with smaller density differences become easier to find due to increased contrast. For example, in liver examinations, the window width can be appropriately reduced to facilitate the detection of lesions with lower density differences; on the other hand, If the window width is increased, the contrast of the image will be reduced, the layers will be richer, and the image will look softer, but lesions with smaller density differences are not easy to observe. In the CT examination of the abdomen, appropriately widening the window position can make a difference in the density of fat and gas in the abdomen. In clinical work, the window width and window level of the CT image should be adjusted appropriately according to the specific situation, so that more diagnostic information can be obtained. Of course, this adjustment is limited.
5 resolution
Image resolution is an important index to measure the image quality of CT equipment, which mainly includes spatial resolution, density resolution and time resolution.
1. Spatial Resolution
The minimum limit of the spatial geometric size of the adjacent objects that can be distinguished in the image, that is, the ability to distinguish fine structures in the image. The spatial resolution of an image is directly proportional to the number of pixels in a unit area. The larger the number of pixels, the higher the spatial resolution.
2. Density Resolution
The minimum limit of the discernible density difference in the image, that is, the ability to distinguish subtle density differences in the image. The density resolution of an image is also related to the number of pixels per unit area. Under other conditions unchanged, the larger the number of matrices, the smaller the volume of each pixel, the fewer the number of light quanta received, and the lower the density resolution. .
Comparing digital imaging equipment such as CT with ordinary plain film, it can be found that the number of matrices of CT and other equipment image is limited. CT usually uses a 512×512 matrix, while each pixel of ordinary plain film is a small silver salt particle. Far larger than digital imaging equipment. In this way, the digital imaging methods, including CT, MRI, CR, etc., actually increase the density resolution and reduce the spatial resolution compared with the traditional plain film.
3. Temporal Resolution (Temporal Resolution)
Refers to the maximum number of frames of images that the device can collect per unit time, which is related to the performance parameters of the device, such as acquisition time, reconstruction time, display mode, continuous imaging capability, etc. During the examination of the lesions of the abdomen parenchymal organs, it is often necessary to perform an enhanced examination. After the enhancement, a continuous and rapid multiphase scan can be performed to obtain more information. Therefore, the time resolution of the device, that is, the scanning speed and continuous scanning capability of the device, is essential for the inspection of moving organs and body organs.
6 Partial Volume Phenomenon
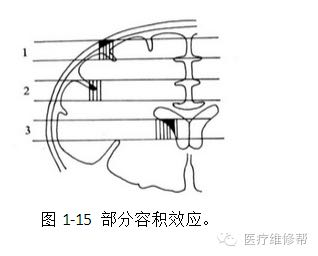
In the layered imaging method, if the same layer contains two or more substances of different densities, the two substances walk and overlap each other in the same layer, that is, when the same voxel contains more than two tissue components (Figure 1-15) , The CT value of this voxel cannot reflect any kind of substance, in fact it is the average of CT values of various tissues. For example, when a voxel contains both bone and muscle, its CT value may be similar to that of muscle, but in fact the voxel does not contain muscle tissue. Therefore, the CT value of small low-density lesions in the high-density zone is often high, and the CT value of small high-density lesions in the low-density zone is often low. This must be paid attention to during clinical observation.
7 reconstruction (reconstruction), retrospective reconstruction (retrospective reconstruction) and reconstruction (reformation)
Reconstruction is to calculate the CT value or density of each voxel in the scan (transverse) plane through a special mathematical algorithm, such as back-projection or Fourier method, from the raw data collected by the detector in the CT scan Value, forming the required digital matrix and (cross-sectional) CT image.
Retrospective reconstruction refers to reconstructing the raw data obtained from the scan in order to better show the fine structure of the image, changing and selecting the best field of view size, field of view center and matrix The number, according to the need to select specific algorithms, such as bone, soft tissue, details or standards, etc., multi-slice spiral CT can also change the layer thickness and number of reconstructed images, thereby improving the density resolution between the tissues, making the image clearer, Delicate and soft, improve sensitivity to fine structures. Commonly used in the display of ossicular chains in the temporal bone, nodules or fine structures in the lung, and pituitary lesions.
Reformation refers to the reconstruction of cross-sectional CT images, through computer technology to perform further post-processing on all or part of the scan level, using different directions and different display technologies to display the anatomy in multiple angles and multiple ways Structure and lesion range, commonly used post-processing reorganization methods include multi-plane reorganization, surface cover display, volume reproduction and virtual endoscope, etc. These different display technologies can make up for the shortcomings of CT cross-sectional display, and visually and stereoscopically display anatomical structures or lesion shapes from different directions.
8 pitch (Pitch)
After the emergence of spiral CT, due to the adoption of a new scanning method of reconstruction algorithm, the distance of the bed moving per revolution of the tube during the scanning process is not necessarily the same as the thickness of the layer. The distance of the bed can be equal to, less than or greater than the thickness of the layer. . In order to measure the speed of movement of the examination bed during the inspection process, an evaluation index-pitch is set. Initially it is defined as the ratio of the distance moved by the tube in one revolution of the bed to the layer thickness or the width of the quasi-value. In a single-slice spiral CT device, the layer thickness and the width of the quasi-scaler are the same, so no matter which one is used, they are the same.
With the advent of multi-layer spiral equipment, especially with different CT equipment such as 4-layer, 16-layer and even 64-layer, the layer thickness and the width of the quasi-value are very different among the above-mentioned equipment. In order to facilitate the comparison of the pitch index among different types of equipment, the pitch is redefined as:
Pitch = the distance moved by the bed per 360º/the width of the quasi-value
In this way, no matter what type of CT equipment, the typical pitch value is between 0 and 2. If in
In the scanning process, increase the pitch and adopt a scanning method with a pitch greater than 1, that is, if the distance of the moving bed is greater than the width of the quasi-scaler, the scanning speed will be improved but the image quality will be reduced; if the pitch is reduced, the scanning method with a pitch less than 1 is adopted. That is, the distance of the moving bed is smaller than the width of the quasi-scaler, although the scanning speed will slow down, the image quality will be improved.
9 Bolus Injection
A bolus injection refers to the rapid injection of contrast medium into a blood vessel. The injection speed per unit time is slightly higher than the blood flow of the blood vessel during the same period, so that all blood in the local blood vessel can be replaced by the injected contrast medium. By adopting the injection method of bolus injection, the concentration of the contrast agent in the artery can reach the peak in a short time, so that the enhancement behavior and characteristics of the lesion can be better observed, and the injection time is too long. Possible interference.
10 artifact (Artifact)
Artifacts refer to the fact that the actual situation during scanning is inconsistent with a series of assumptions in the process of reconstructing the image, and the resulting image does not conform to the actual situation. Common artifacts in CT include the following: ①Motion artifacts: The movement artifacts caused by the movement of the patient during scanning, which are generally strip-shaped low-density shadows; ②Beam hardening artifacts: When X-rays pass through high-density Structures or substances, such as occipital tuberosity, teeth, postoperative silver clips, etc., will cause changes in the X-ray penetration characteristics, which will cause errors in the attenuation calculation in the subsequent calculation and reconstruction process, which can be radial or striped High-density or low-density shadows; ③Machine failure artifacts: There are many causes and types of such artifacts. If the detector works abnormally, it can cause ring-shaped or concentric artifacts.